Extending the lifespan of N95 masks
Researchers are working to better understand how decontamination procedures might affect the structure and potential reuse of N95 masks.
By Erin MatthewsA CT scan of an N95 mask, taken using the BMIT beamline at the CLS, shows the fiber structure within the respirator.
Through a collaboration between the Canadian Light Source (CLS) and the Vaccine and Infectious Disease Organization-International Vaccine Centre (VIDO-InterVac)—both national research facilities at the University of Saskatchewan (USask), scientists hope to understand the structural changes happening inside N95 respirator masks after being sterilized for reuse.
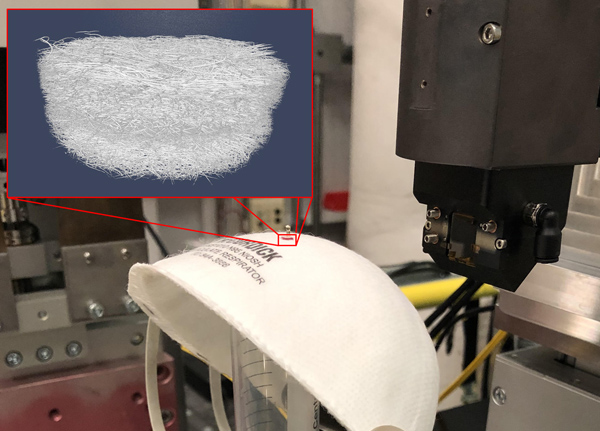
Cutting-edge techniques unique to the CLS enable the team to analyze minute details in the masks that would be impossible to see with other methods. CLS Industrial Scientist Toby Bond is using X-rays produced by the synchrotron to see the tightly woven, microscopic fibers that are crucial to the filtering power of N95 respirators.
N95 respirators get their name from their ability to filter at least 95 per cent of particles circulating in the air. These particular masks are used by frontline healthcare workers for protection against COVID-19.
However, N95 masks that were intended for one-time use were in short supply globally during the height of the pandemic this spring, and continue to be chronically unavailable in most parts of the world. As a result, health care agencies and researchers have been looking for ways to sterilize masks for reuse to help ensure an emergency supply.

While previous research has found that certain methods work better at maintaining the integrity of the masks following decontamination, Bond and colleagues want to understand why this happens and how to extend the lifespan of these critical masks.
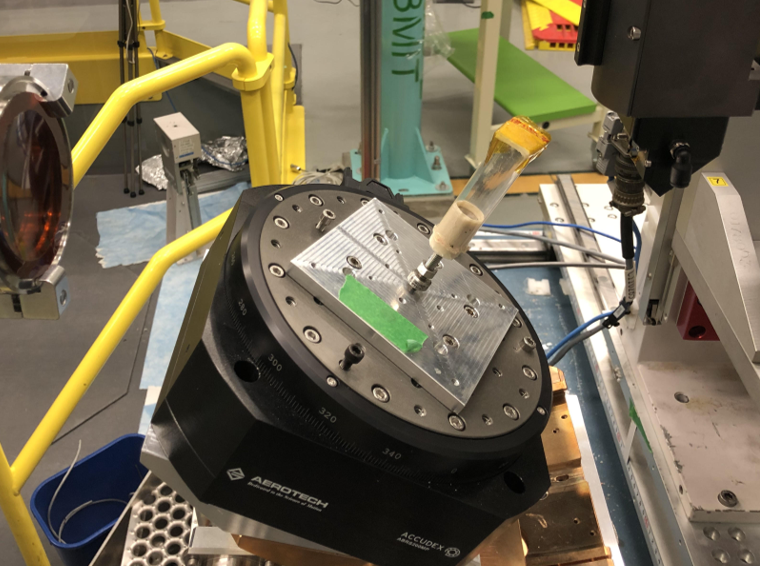
“We want to use the unique tools we have at the CLS to look at the fibers that actually do the filtering,” Bond said. “We use a specialized X-ray microscope to take tiny CT scans before and after exposing the N95 masks to different decontamination protocols. Previous research has shown that certain methods work better than others, but we don’t currently know what’s going on inside the mask at a microscopic level.”
Bond is working to determine why the N95 mask fibers degrade. This information would enable manufacturers to design more resilient masks and help the medical industry move towards personal protective equipment that is deigned to be reusable.
“One thing that’s unique about a synchrotron CT scan is that we can scan a tiny fraction of the mask at high magnification without having to cut small pieces out of it. This is what allows us to do before-and-after imaging, since we can decontaminate the mask in its real-world environment without altering it,” Bond added.
One method for decontaminating N95 masks, called vaporized hydrogen peroxide (VHP), is used to sterilize rooms and equipment in VIDO-InterVac.
“With the outbreak of the pandemic and the recognized potential worldwide shortage of respirators, we were approached by the Saskatchewan Health Authority (SHA) to investigate the possibility of using VHP decontamination on N95 respirators to mitigate a potential shortage,” said VIDO-InterVac Biosafety Officer Tracey Thue.
To date, VIDO-InterVac has sterilized more than 13,000 masks. Studies have demonstrated that N95 masks can undergo multiple VHP decontamination cycles without affecting mask integrity.
When CLS Laboratory Coordinator Burke Barlow suggested that the two groups collaborate, Thue offered to run three styles of N95 respirators through their VHP system for Bond’s research. Bond compared the VHP-treated masks to others that he had treated with Moist Heat Incubation (MHI) and autoclaving.

Autoclaving is a common decontamination method that uses hot pressurized steam to sterilize medical devices, however it is the most damaging method and certain masks do not survive even one autoclave sterilization cycle. MHI is gentler than the autoclave, but the masks still become less effective after repeated cycles. VHP is considered to be the best method for decontamination of N95s, but it requires specialized equipment that is not widely available in hospitals.
Bond and his colleagues are using the BMIT beamline at the CLS, a one-of-a-kind tool in North America, to image the inside of the masks in three dimensions without damaging them. The researchers can then look at the structure of individual fibers in the masks to see how they change during decontamination. They can identify shifts in mask fibers as small as a few microns, which is a measurement much smaller than the width of a human hair.
Analyses over the next few weeks will help clarify what effect these shifts have on the performance of the mask. Aerodynamic and fluid simulations conducted at the CLS will help show how the changes in mask fiber structure affect air flow.
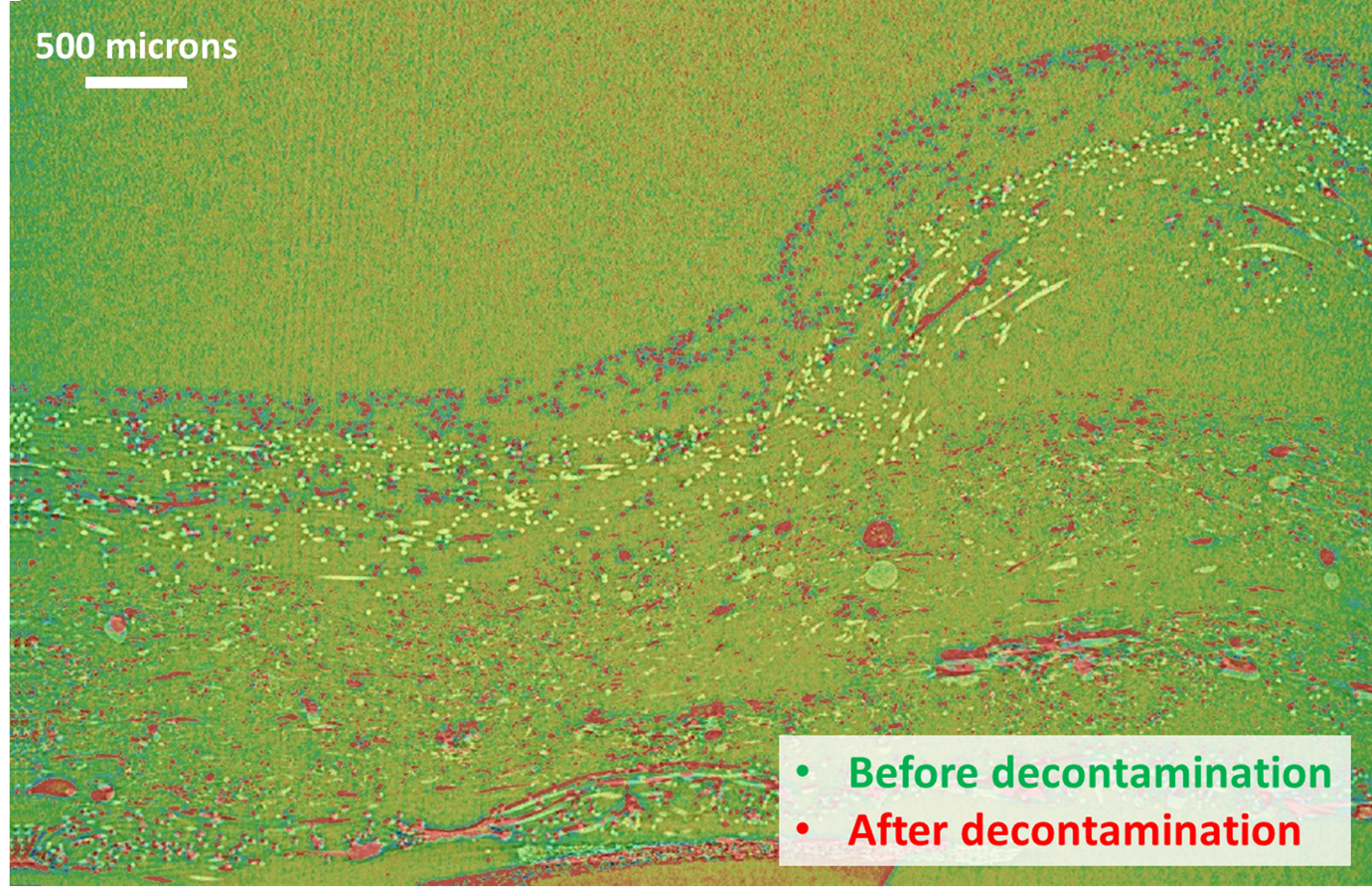
“Preliminary results show there is a gradual unravelling of the fibers during repeated exposure to MHI in some masks,” said Bond. “This is in contrast to autoclaving the masks, which immediately causes a very significant unravelling after a single decontamination.”
“In some cases, this unravelling doesn’t affect the filtration, but it does affect the overall structure of the mask, causing it to fit poorly and no longer seal properly to the user’s face,” he added. “This indicates that manufacturers could potentially make an autoclavable mask by changing the structural parts of the mask and leaving the filtration layer as it is.”
“In terms of Toby’s research at the CLS, being able to go down to the microscopic level and visualize changes in the material or lack there-of is another valuable piece of information,” Thue said.
Bond emphasized that it’s not just tools and equipment that makes this kind of research possible at the CLS, but also the access to the vast research network at USask.
“The CLS is a fantastic place to do research like this, since we’re a national facility with a broad network of researchers,” said Bond. “We’ve been able to work with our colleagues at VIDO-InterVac (which is just down the road on the USask campus), and we also have contacts in industry and academia who work in this sector that have helped us with the experiments.”
The CLS and VIDO-InterVac are two of Canada’s top science facilities. Both receive funding from the Major Science Initiatives (MSI) Fund of the Canada Foundation for Innovation.
For more information, contact:
Victoria Schramm
Communications Coordinator
Canadian Light Source
306-657-3516
victoria.schramm@lightsource.ca
